Microbiomes — Hope OR Hype?
20 March, 2020Although we have long known about the existence of microbes—the tiny bacteria, fungi and archaea that live all around us, on us, and in us—interest in how the microbiome might impact human therapeutics has become a hot topic in research only recently.
In light of our March 2017 web panel discussion, we sat down with Dr. Ravi Kiron, Managing Partner at Biopharm Strategy Advisors and moderator of the webinar, to find out whether this area could revolutionize the healthcare industry of the future or whether we are treading on dangerous ground that we know little about.
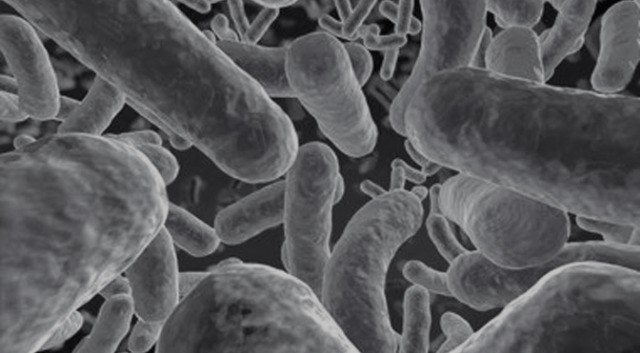
 Before we dive into our interview with Ravi, it's essential to understand microbiome as a field of study. A microbiome is the collection of microbes or microorganisms that inhabit an environment creating a sort of “mini ecosystem.” The human microbiome is made up of communities of symbiotic, commensal and pathogenic bacteria (along with fungi and viruses) all of which call our bodies home. Some of these bacteria—the commensal—are simply along for a free ride, while others—the symbiotic bacteria—offer a mutually beneficial relationship. Always lurking, although in much smaller numbers, are pathogens—disease-causing opportunistic microbes. Pathogens, however, do not always cause disease, and some in fact have beneficial effects.
Before we dive into our interview with Ravi, it's essential to understand microbiome as a field of study. A microbiome is the collection of microbes or microorganisms that inhabit an environment creating a sort of “mini ecosystem.” The human microbiome is made up of communities of symbiotic, commensal and pathogenic bacteria (along with fungi and viruses) all of which call our bodies home. Some of these bacteria—the commensal—are simply along for a free ride, while others—the symbiotic bacteria—offer a mutually beneficial relationship. Always lurking, although in much smaller numbers, are pathogens—disease-causing opportunistic microbes. Pathogens, however, do not always cause disease, and some in fact have beneficial effects.
 Interest in this field of research has exploded in recent years thanks to advances in genomic and big data analysis. We are seeing widespread efforts to bring private companies, academia and investors together in order to advance our understanding of the human microbiome and how it could potentially be considered a therapeutic area target for focused R&D by global biotech and pharma companies.
Interest in this field of research has exploded in recent years thanks to advances in genomic and big data analysis. We are seeing widespread efforts to bring private companies, academia and investors together in order to advance our understanding of the human microbiome and how it could potentially be considered a therapeutic area target for focused R&D by global biotech and pharma companies.
Q: What is microbiome? Is it a field? A therapy?
A: Our current understanding of the microbiome is still in its infancy. It's unclear whether it would fall into its own specific therapeutic area right now. We are beginning to appreciate the impact this exploration could have on different kinds of disease outcomes and as such it could be very significant. The most common perturbations or maladies that people associate with the human microbiome is that of Traveler's Diarrhea or other gastrointestinal upsets that we are susceptible to as a reaction to the foods we eat or the infections we get exposed to in our lives. There are other more serious maladies, such as acute and chronic GI related complications, such as IBS, IBD, Crohn's Disease and Ulcerative Colitis. These illnesses that are directly connected to microbiota changes are only the tip of the iceberg. There is ongoing research that suggests that the microbiome can affect the immune system, diabetes and obesity, cardiovascular, and is even capable of controlling or modifying brain health. So, we have a long way to go and continued future research will undoubtedly help to classify it as a new therapeutic area or a field of study that has far-reaching implications.
Here is an interesting factoid: There are 100 thousand billion bacteria in each of us that codify over three million genes, and there are 1000 times more bacteria in each one of us than there are stars in our galaxy. So, there is a microcosmos within the macrocosmos (watch the AmazonPrime show on Gut – The Second Brain). Essentially, there are 2 to 5 pounds of bacteria in each of us—which account for 30% of our caloric intake, since they convert the food we ingest into energy for the body. What this essentially means is that each of us are an ecosystem with more bacteria cells than human cells.
Q: How did you get interested in microbiome?
A: Many years ago, I read an article about Eric Alm, who was then a Professor at MIT. The article outlined an experiment that Professor Alm and one of his graduate students, Lawrence David, participated in for over a year where they recorded everything they ate and collected stool samples every time they defecated. They kept detailed records of everything that went into their bodies and collected and froze samples of everything that came out, which is a feat on many different levels. I mean, who would do that for an entire year! All of these samples have and are continuing to be re-analyzed (through microbiology and gene sequencing) with new tools and algorithms that have been built specifically for this purpose. Some of the results have been published and are quite fascinating.
The Human Genome Sequencing project was completed in 2003, and we are only now beginning to understand the implications of our expanding knowledge of the human genes that control our lives. Now we realize that there are thousands of other genes from the microbiome within us that are most likely having an effect on our lives. So, gaining a greater understanding of what else is going on in the human body in terms of the microbiome seems like the next logical step. The microbiologist within me (I have an MS in Microbiology) was very intrigued and that was my introduction to the microbiome. Over the years, I have continued to follow the microbiome field. More recently, I had the opportunity to work with Clasado BioSciences, who are one of the leading experts in the field of gut-mediated wellness.
The other news that happened around the time that the microbiome was gaining visibility was that Dr. Craig Venter, who is known for being the first to sequence the human genome, had developed an interest in the earth's microbiome. As part of his Global Ocean Sampling expedition, he and his team collected water samples from the deep sea and filtered them to capture the unique microorganisms at each location, with the goal of unlocking the secrets of the oceans through a study of its microbiome.
Q: We’ve been talking about the human microbiome, but the deep sea?
A: Yes. Interestingly, there are five classifications of microbiomes.
The first is the human microbiome. When we talk about the human microbiome, we are mostly referring to the gut, although there are specific microbiomes that exist in a person’s oral cavities such as the nose, the ears, the throat (which is an extension of the gut and the anus), the urogenital region, and as you know, the surface of our skin.
The second microbiome is in the building and the air that is in it. People in the building are constantly sharing their own individual microbiota with everyone else, through breathing, speaking, sneezing, physical contact and other exchange of body fluids. The building ecosystem is important for managing public health.
 The third is the soil microbiome. Here we are referring to the soil microflora that vary in different parts of the world and that are very important to plant growth and maintenance. An example of the soil microbiome are the nitrogen fixing bacteria in the soil. These are transferred to humans when we eat the plants and associated products.
The third is the soil microbiome. Here we are referring to the soil microflora that vary in different parts of the world and that are very important to plant growth and maintenance. An example of the soil microbiome are the nitrogen fixing bacteria in the soil. These are transferred to humans when we eat the plants and associated products.
The fourth is the aquatic microbiome, which is subject to natural variation and is influenced by environmental factors such as light, temperature, pH, salt concentration and the multitude of microorganisms that exist and contribute to the eternal circle of life. An example of extreme environment microorganisms in water are the thermophilic bacteria found in the hot springs and geysers in Yellowstone National Park.
The last is the outer space microbiome, of which we don’t know very much about.
Q: Could disturbing the microbiome have negative effects?
A: Absolutely. That’s what happens with extreme antibiotic usage that can lead to a disrupted ecosystem that can stimulate expansion of a bad species of a bacteria called Clostridium difficile (C. diff) causing infections. In 2011, there were more than 450,000 cases of C. diff. infections in the United States, causing 29,000 deaths. We don’t hear a lot about it because a lot of these cases get rationalized as another issue, such as a heart attack or something else. So yes, there can be both positive and negative effects.
Q: Is it common to get an infection through the digestive system?
A: It’s very common. According to data collected through the New York Travel Clinics, twenty million Americans visit Mexico every year and 40% of them get some kind of GI sickness as a result of unclean water or tainted food. You’ve undoubtedly heard of Montezuma’s Revenge. In India it’s referred to as Delhi Belly.
Q: When did the microbiome field start gaining traction?
A: I would say that real interest and visibility into the human microbiome began in 2012. I don’t recall exactly what triggered the interest, but I can tell you that the microbiome made the cover of Science, Nature, Scientific American and The Economist, all in 2012.

Q: Have there been any microbiome therapies approved?
A: There are microbiome related therapies, such as fecal transplants that have been proven to successfully treat C. diff. infections, but nothing so formal as having FDA approval. There are, however, other published case reports or individual studies that are employing fecal transplants to treat IBD, IBS, chronic fatigue syndrome and multiple sclerosis, among others. The challenge is that of streamlining treatment, such that it would fall under the confines of the FDA's stringent guidelines for safety and efficacy, with any new Investigational New Drug. However, I believe that all this may be poised for a change as large pharmaceutical and biotech companies begin to eye the medical and financial potential of manipulating interactions between humans and the bacteria that live in or on the body.
 Q: For a long time there’s been a focus on supporting digestion in various ways. But the interest in the microbiome seems to go beyond that. Now we’re hearing talk of impacting brain health, modulating infections, or even using the microbiome to trigger the immune system in cancer patients. Is that accurate?
Q: For a long time there’s been a focus on supporting digestion in various ways. But the interest in the microbiome seems to go beyond that. Now we’re hearing talk of impacting brain health, modulating infections, or even using the microbiome to trigger the immune system in cancer patients. Is that accurate?
A: Yes. It’s a very nascent field, but there are some implications that seem obvious. We take drugs for diseases and most of these drugs are broken down in the stomach. If we could control the functions of beneficial bacteria in the stomach and increase the effectiveness of how drugs are broken down in the stomach, then it might be possible to take much lower doses of those drugs. Lower doses translate into reduced side effects. There is also speculation and insights that are being developed about the microbiome generating molecules that reduce inflammation and play a crucial role in the induction, basic development, training and function of our immune system, with implications in innovative immuno-oncology or other cancer therapies. There is also emerging evidence connecting mental illnesses with neuropsychiatric conditions such as Alzheimer's Disease, Parkinson's Disease, autism, schizophrenia and gut dysbiosis (gut microbiome-host maladaptation). Researchers have also identified certain intestinal bacterial groups that play a role in human obesity. Current research and development efforts are bound to take us much further.
Q: Has there been work done to identify all the bacteria that lives in the gut?
A: There are several academic groups who have isolated and microbiologically identified every species of bacteria, fungi, viruses and phages and are following them with a view to correlating human consumption and lifestyle changes on the microbiome species resident in the gut over time. This is a massive task and requires a lot of time, funding, and teams of researchers and labs, since this is an individual analysis. Researchers have also classified our microbiomes into three enterotypes (like blood serotype grouping). These enterotypes are independent of geography, race, sex and age, so this makes it even more challenging a task to map each person and devise a therapy specific for that individual. Ultimately, our expanding interest and study into the microbiome will help us understand the basic question of whether changes in the microbiome cause disease or whether disease causes changes in the microbiome. Lawrence David (Professor Alm's graduate student mentioned earlier) had salmonella poisoning during the one-year experimentation and that changed his microbiome. He was treated and recovered from the salmonella poisoning, but his microbiome remained altered. All in all, there really is a lot more research and understanding that needs to happen before we can begin to leverage our new understanding of the human microbiome.
Q: Who are the most active players in the microbiome space right now?
There are many academic and industry groups that are active in this space. A few investors have also bought into the microbiome hope or hype, and there are several startups that are enhancing our understanding of this area. In the web panel discussion, you can hear from three of these exciting startups—MatriSys Biosciences, Whole Biome and Second Genome.
Other leaders are people such as Craig Venter. He has his own organization called the J. Craig Venter Institute (JCVI), and they are really pushing the boundaries of our understanding of the microbiome research forward. Also Rob Knight, who is the co-founder of both the American Gut Project and the Earth Microbiome Project. His lab’s research involves the development of laboratory and computational techniques to characterize the microbiomes of humans, animals and the environment. A team of researchers at Novartis and the Broad Institute of MIT and Harvard are exploring whether the microbiome can be used to prevent and treat disease. Bristol-Myers Squibb is collaborating with Paris-based Enterome Biosciences in discovering new treatments for patients with cancer by focusing on the gut microbiome. Janssen has established its own Microbiome Institute. And, of course, there is Eric Alm, now at Duke, who is continuing in his quest to decipher his own microbiome and apply those learnings to streamlining the study of each individual microbiome.
Also, the hype that’s happening right now is serving to push things forward. Just like many years ago when adding a ".com" to the end of your company name immediately resulted in a 40% increase in stock value. Microbiome is something like that, although one can also visualize the study of the microbiome to the image of ten blind men touching an elephant and declaring their findings. Investors and the public are seeing this as a new investment opportunity. Today's informed public is also interested since this is something that will affect every human being on the face of the planet. Large pharma is slowly coming around, and I think eventually they will be a driver.
Ultimately, it will probably take someone showing a clear cause/effect relationship between changing the microbiome resulting in efficacy in treating or preventing some disease paradigm. Let’s hope for that day to come soon, our stomachs and our microbiomes that are part of us, will thank us.
Request a recording of the web panel discussion or a white paper on "Microbiome: Hope or Hype?"
For the web panel discussion, Ravi was joined by:
- Mark S. Wilson, President and CEO of MatriSys Bioscience, Inc.
- Colleen Cutcliffe, CEO and Co-founder of Whole Biome
- Mohan Iyer, Chief Business Officer of Second Genome
